Helena O. Taylor MD, PHD, FACS & Stephen R. Sullivan, MD,MPH,FACS
Facial Trauma can result in open wounds, broken bones, scars, or facial asymmetry. Reconstruction requires meticulous repair of all injured structures by an experienced surgeon.
Dr. Taylor and Dr. Sullivan are both fellowship trained in Craniomaxillofacial Surgery and are former co-directors of the Division of Craniofacial Surgery at Brown University. Because of their experience, they have been named faculty members for AOCMF to teach other surgeons the principles of proper facial fracture repair and reconstruction. They have published extensively on their experience in helping patients with traumatic or acquired facial injuries and have educated colleagues nationally and internationally. If you have a new facial injury or a past history of an injury with ongoing problems, please contact us for an evaluation and carefully planned approach to restore your face. Most operations related to facial trauma are covered by insurance.
We enjoy looking after patients with a broad range of problems in our practice.
We particularly enjoy restoring facial form and function after trauma. With many years of working at high volume trauma centers, we feel very comfortable performing complex reconstructions of bony and soft tissue injuries of the face and head, taking advantage of the latest technologies. These include nasal, mandibular, maxillary, orbital and frontal bone fractures. We hope you wear your helmet and never need our services. But if you do, we will do our best to put things back where they belong.
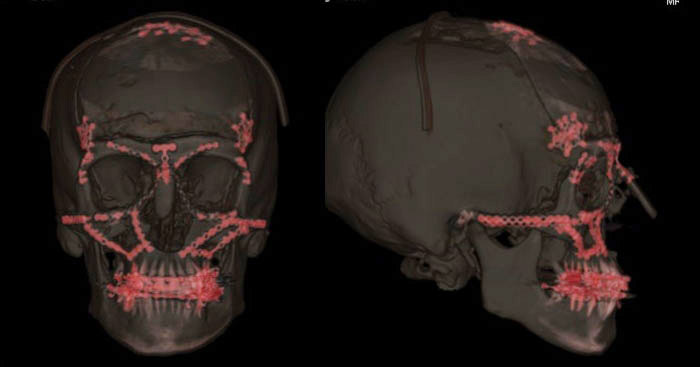
Our goal is to always deliver the best craniofacial surgery Boston has to offer. When indicated, we will use the latest technology to rebuild facial structures, including 3D imaging, 3D presurgical planning, and 3D printing. Most facial fractures are repaired with mini or microplates and screws made of titanium. While some doctors may shave a patients hair or use extensive incisions, Dr. Taylor and Dr. Sullivan will conceal incisions inside the mouth or eyelid creases and don’t usually need to shave any hair for even the most complicated facial reconstruction operations.
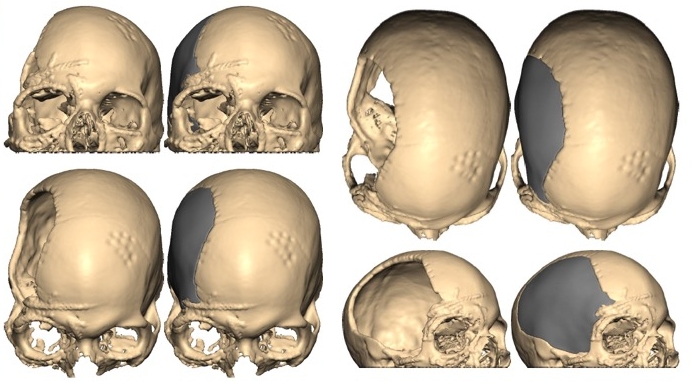
Restoring normal appearance of skull and facial profile while protecting the brain, eyes or critical structures is of primary importance when repairing facial fractures.
Dr. Taylor and Dr. Sullivan use technology such as 3D preoperative planning and 3D printing to customize treatment plans for our Boston craniofacial surgery patients. Especially those patients who have suffered cranial or facial deformities because of previous operations, trauma, cancer or congenital anomalies such as craniosynostosis. These images show a patient with extensive facial fractures and skull defect who underwent reconstruction and cranioplasty following careful 3D planning and 3D printing of a custom craniofacial implant with Dr. Sullivan and Dr. Taylor.
Not all facial fractures require surgery.
But when the bones are significantly displaced and/or mobile, we will often recommend open reduction and internal fixation. We expose the fractures through well concealed incisions, put the bones back in their correct position, and secure them with titanium microplates and screws. While the risks of this type of craniofacial surgery include residual asymmetry, infection, damage to facial nerves, and need for hardware removal, these complications are thankfully rare.
Our goal is to restore things to their pre-injury state with the lowest risk to the patient. Dr. Taylor and Dr. Sullivan conduct research, publish their experience with facial fracture treatment, and use the latest technology to reconstruct the face, including 3D planning, 3D printing, and titanium miniplate fixation (above images show plating in red following repair of extensive pan- or complete facial fractures.
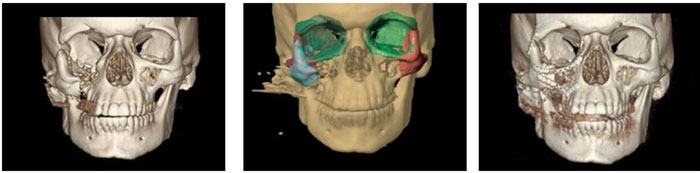
This is an example of a 3D CT scan demonstrating a right zygomaticomaxillary complex (ZMC) or “tripod" fracture.
On the left the image demonstrates the severe inferior position of the ZMC due to the downward pull of the masseter muscle. Over time, the patient became severely disfigured. Dr. Taylor and Dr. Sullivan used the latest technology to reconstruct the face, including 3D planning, 3D printing, intraoperative CT scan and intraoperative image guidance.
The center image demonstrates the goals for the craniofacial surgery with this technology. On the right, the facial bones have been reconstructed and repaired with titanium miniplates for rigid internal fixation. Incisions are hidden inside the mouth and in a wrinkle in the upper eyelid and lower eyelid. Their novel use of this technology was published: Morrison CS, Taylor HO, Sullivan SR. Utilization of intraoperative 3D navigation for delayed reconstruction of orbitozygomatic complex fractures. Journal of Craniofacial Surgery. 2013;24(3):e284-286.

Use of intraoperative computed tomography in complex craniofacial trauma: an example of on-table change in management. Morrison CS, Taylor HO, Collins S, Oyelese A, Sullivan SR. Craniomaxillofac Trauma Reconstr. 2014 Dec;7(4):298-301. doi: 10.1055/s-0034-1378179. Epub 2014 Jun 10. PMID: 25383151
Morrison CS, Taylor HO, Sullivan SR. Utilization of intraoperative 3D navigation for delayed reconstruction of orbitozygomatic complex fractures. Journal of Craniofacial Surgery Boston. 2013;24(3):e284-286.
Interdisciplinary Management of Minimally Displaced Orbital Roof Fractures: Delayed Pulsatile Exophthalmos and Orbital Encephalocele. Ha AY, Mangham W, Frommer SA, Choi D, Klinge P, Taylor HO, Oyelese AA, Sullivan SR. Craniomaxillofac Trauma Reconstr. 2017 Mar;10(1):11-15. doi: 10.1055/s-0036-1584395. Epub 2016 Sep 15. PMID: 28210402
Restoring alignment of teeth is one of the primary goals with repair of facial fractures. Dr. Taylor and Dr. Sullivan are both fellowship trained craniofacial surgeons and board certified plastic surgeons who are experienced with complex facial reconstruction.
Post-injury prophylactic antibiotics likely provide no benefit in maxillary, zygomatic, or mandibular condyle fractures. Closed isolated anterior table frontal sinus fractures and orbital fractures also rarely become infected and likely do not require antibiotics.
Some fractures, for example mandibular body and angle fractures, particularly those that penetrate a tooth root can have infection rates up to 30%. Frontal sinus fractures with disruption of the frontonasal duct may have a 16% infection rate even after surgical treatment. A short course of antibiotics in conjunction with chlorhexidine mouth rinses may be warranted in such fractures.
In terms of perioperative antibiotics, it seems reasonable to give a first generation cephalosporin for no more than 24 hours for low risk, closed facial fracture repairs. Ballistic injuries, grossly contaminated open facial fractures, nasal fractures with packing in place, and infected mandibular fractures may require a 4-5 day postoperative course of antibiotics.
Call Today 617.492.0620
To schedule a private consultation with Dr. Taylor or Dr. Sullivan, please call the office or request an appointment using our form. We welcome your visit and your questions.
300 Mount Auburn St. Ste 304, Cambridge, MA 02138





