Named Among the Best Plastic Surgeons in Boston
Helena O. Taylor MD, PHD, FACS & Stephen R. Sullivan MD, MPH, FACS
Breast Reconstruction is performed after treatment for breast cancer.
With 1 in 8 women in the United States having a diagnosis of breast cancer, breast reconstruction is one of the most common operations performed by plastic surgeons. Although most women will have breast conservation therapy, some will require mastectomy (removal of the breast) or elect to have mastectomy because of a genetic susceptibility with high risk for breast cancer such as a BRCA gene mutation. In addition to removing the breast, some women will also have removal of the nipple and areola, while others may be a candidate for nipple sparing mastectomy, which means that the breast tissue is removed while the skin, nipple and areola remain.
Some women will elect to have breast reconstruction following mastectomy. Boston Mass plastic and reconstructive surgeons Dr. Taylor and Dr. Sullivan have published their experience with breast reconstruction and are able to work together as a team to provide reconstruction tailored to each woman's needs. The timing of reconstruction can be immediately after removing the cancer or delayed to allow a safe recovery from the first procedure. Dr. Taylor and Dr. Sullivan provide support and education until the timing for breast reconstruction is right for you.
The type of breast reconstruction varies: direct-to-breast implant, tissue expander followed by breast implant in a second stage, or using of a woman's own tissue from elsewhere on her body. The type and timing of breast reconstruction are carefully discussed with each woman, so we can understand and support your wishes and needs.
When a woman's own tissue is used, common locations are the tummy tissue and back tissue. The tummy tissue can be known as a transverse rectus abdominis myocutaneous flap (TRAM flap). This operation is very similar to a tummy tuck, and involves moving skin, fat and and a small area of muscle from the abdomen to make a new breast.
A TRAM flap allows breast reconstruction as well as simultaneous tummy tuck. A related form of tummy tissue reconstruction is the deep inferior epigastric peforator flap (DIEP flap), which moves only skin and fat while preserving the abdominal muscles. Back tissue, known as a latissimus dorsi myocutaneous flap, moves skin, fat and muscle from the back to make a new breast and is usually combined with a breast implant.
Breast reconstruction performed in the past can also be revised using the methods discussed above as well as fat grafting to correct smaller contour deformities. Dr. Taylor and Dr. Sullivan will spend time with you to carefully select an approach for your Boston breast reconstruction, with careful consideration of your overall health and recovery.
With Breast Implant

Dr. Sullivan and Dr. Isik have conducted research and published information on breast reconstruction (Plastic and Reconstructive Surgery. 2008;122(1):1493-1498), including information on the timing of implant based breast reconstruction. This patient underwent delayed reconstruction with a tissue expander followed by a breast implant. Preoperatively (left) after mastectomy and radiation for breast cancer. Postoperatively (right) after tissue expansion and exchange for a permanent breast implant and before nipple and areola reconstruction.
With DIEP flap

Dr. Sullivan and Dr. Isik have conducted research and published information on breast reconstruction (Plastic and Reconstructive Surgery. 2008;122(1):1493-1498), including information on the timing of using a woman's own tissue, known as autologous tissue breast reconstruction. This patient underwent delayed breast reconstruction with tissue from the abdomen known as a deep inferior epigastric artery perforator flap (DIEP flap). Preoperatively (left) after mastectomy and radiation for breast cancer. Postoperatively (right) after DIEP flap and nipple and areola reconstruction.
Breast reconstruction methods include placement of a breast implant versus use of a woman's own tissue from elsewhere on her body, or a combination of both.
Breast implants can be saline (salt water) or silicone gel. Silicone gel has been found to be a safe and more natural feeling breast implant reconstruction.
Dr. Taylor and Dr. Sullivan work with many companies including Mentor, Allergan, and Sientra to optimize your breast implant options. Additional options for silicone gel include a smooth versus a textured implant and a round versus a shaped implant.
Smooth breast implants are the most common form used in breast reconstruction Boston plastic surgeons Dr. Taylor and Dr. Sullivan recommend them as textured implants have been found with increasing frequency to be associated with breast implant-associated anaplastic large cell lymphoma, or BIA-ALCL. BIA-ALCL is not breast cancer, it is a type of non-Hodgkin’s lymphoma. To decrease your risk, smooth breast implants are recommended and often a Keller funnel is used to decrease exposure to bacteria and risk for infection. If you have a past history of a textured breast implant and have symptoms such as capsular contracture, painful scar or a fluid collection, please consider meeting with Dr. Taylor and Dr. Sullivan to learn more about breast implant removal and exchange.
With DIEP flap

Dr. Sullivan and Dr. Isik have conducted research and published information on breast reconstruction (Plastic and Reconstructive Surgery. 2008;122(1):1493-1498), including information on the timing of using a woman's own tissue, known as autologous tissue breast reconstruction. This patient underwent immediate breast reconstruction with tissue from the abdomen known as a deep inferior epigastric artery perforator flap (DIEP flap). Preoperatively (left) before mastectomy and radiation for breast cancer. The blue marks on the abdomen indicate the location of perforating blood vessels from the the deep inferior epigastric artery. Dr. Sullivan and colleagues have conducted research and published information on the size and location of these vessels as they relate to body mass index (Journal of Reconstructive Microsurgery. 2009;25(4):237-241). Postoperatively (right) after DIEP flap and nipple and areola reconstruction as well as radiation therapy.
With Breast Implant
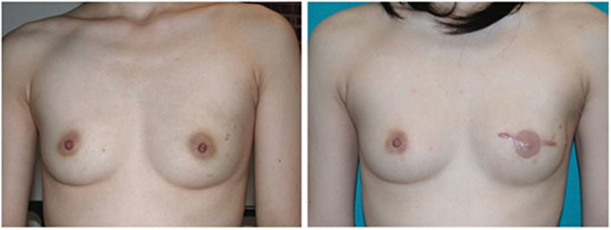
Dr. Sullivan and Dr. Isik have conducted research and published information on breast reconstruction (Plastic and Reconstructive Surgery. 2008;122(1):1493-1498), including information on the timing of implant based breast reconstruction. This patient underwent immediate left breast reconstruction with a tissue expander followed by a breast implant. Preoperatively (left) before mastectomy for breast cancer. Postoperatively (right) after immediate tissue expansion and exchange for a permanent breast implant and soon after nipple and areola reconstruction.
Following mastectomy for breast cancer or prophylactic mastectomy because of increased risk for breast cancer or BRCA gene mutation, you may be a candidate for immediate breast implant placement (silicone gel or saline) or you may have a tissue expander placed with the goal of creating room for a final breast implant placed at a later time.
Working closely with Dr. Taylor and Dr. Sullivan, as well as the breast team, you may consider immediate breast reconstruction at the time of the mastectomy, as shown in the above image published by Dr. Sullivan.
The preoperative photograph (above, left) demonstrates a woman before undergoing left mastectomy and immediate placement of a tissue expander followed by second stage breast implant reconstruction, shown 1 year postoperatively (above, right) at the time of nipple construction and areola tattooing. Some of our Boston breast reconstruction patients can avoid the need for a tissue expander and proceed straight to an immediate breast implant, often with simultaneous internal dermal sling. Nipple sparing mastectomy and immediate breast implant placement is also an increasingly common practice offered by Dr. Taylor and Dr. Sullivan.
Preoperatively, In the week before your operation:
Postoperatively,
Please take your medications as directed by Dr. Taylor or Dr. Sullivan to manage discomfort or symptoms.
You are likely to be given:
You may also be given:
Eat a light diet for 2-3 days and avoid spicy food. Some suggestions to ease abdominal discomfort or indigestion after surgery:
WOUND CARE
ACTIVITY
GENERAL OUTCOMES
It is important to be seen by Dr. Taylor or Dr. Sullivan after your operation. They will see you in follow-up appointments at regular intervals, typically 1 week, 2-4 weeks, 3 months, 6 months, and 1 year or as often as needed post-op. Call to schedule your appointments at Taylor & Sullivan Plastic Surgery office at (617) 492- 0620 between the hours of 8:30 – 5:00 or visit our webpage at www.massplasticsurgeons.com. We are always available for postoperative concerns or emergencies and can be reached through our paging service 24 hours per day at (617) 492-0620.
Download our Breast Lift and Breast Reduction Postoperative Instructions Here.
Call Today 617.492.0620
To schedule a private consultation with Dr. Taylor or Dr. Sullivan, please call the office or request an appointment using our form. We welcome your visit and your questions.
300 Mount Auburn St. Ste 304, Cambridge, MA 02138





